PERIPHERAL ARTERY DISEASE
Causes
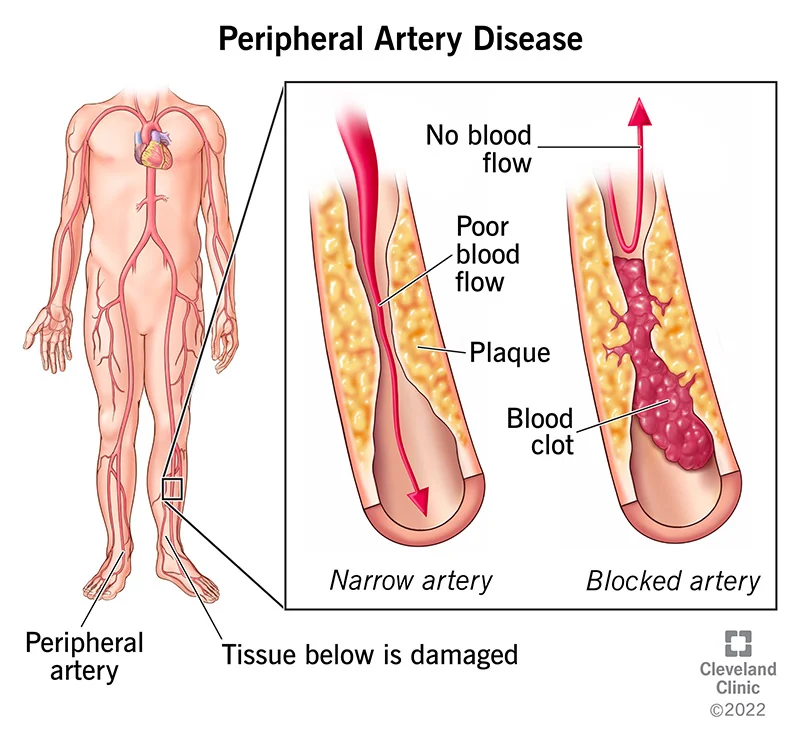
Atherosclerosis is the main cause of peripheral artery disease. Fatty deposits (plaques) build up in your artery walls and reduce blood flow in atherosclerosis. This disease can and usually does affect arteries throughout your body although the heart is usually the focus of discussion of atherosclerosis. Atherosclerosis in the arteries supplying blood to your limbs causes peripheral artery disease. The cause of peripheral artery disease, less commonly, may be blood vessel inflammation, injury to your limbs, unusual anatomy of your ligaments or muscles, or radiation exposure.
Symptoms
Generally, most people with peripheral artery disease have mild or no symptoms. Some people have leg pain when walking (intermittent claudication). The symptoms of intermittent claudication include muscle pain or cramping in your legs or arms that’s triggered by activity, such as walking, but disappears after a few minutes of rest. Pain is localised to the area supplied by the clogged or narrowed artery. Pain in the calf is the most common location.
There is a wide variation in the severity of intermittent claudication, ranging from mild discomfort to debilitating pain. Walk or doing other types of physical activity could be a hard task due to severe intermittent claudication.
Other symptoms of peripheral artery disease include:
- Cramps and pain in your hip, thigh or calf muscles after activity, such as walking or climbing stairs (intermittent claudication)
- Numbness or weakness in leg
- Feeling cold in your lower leg or foot, especially when compared with the other side
- Ulcers on your toes, feet or legs that won’t heal
- Color change of your legs
- Loss of hair or slower hair growth on your feet and legs
- Decreased growth of your toenails
- Shiny skin on your legs
- Absent pulse or a weak pulse in your legs or feet
- Erectile dysfunction in men
Progression of peripheral artery disease can lead to pain that may even occur when you’re at rest or when you’re lying down (ischemic rest pain). Its intensity could be strong enough to disrupt sleep. Temporary relief could be obtained by hanging your legs over the edge of your bed or walking around your room.
DIAGNOSIS
To diagnose peripheral artery disease, your doctor may rely on the following tests:
- Physical exam. On physical examination, your doctor may find signs of PAD such as a weak or absent pulse below a narrowed area of your artery, whooshing sounds (bruits) over your arteries that can be heard with a stethoscope, evidence of poor wound healing in the area where your blood flow is restricted, and decreased blood pressure in your affected limb.
- Ankle-brachial index (ABI). One of the most common tests to diagnose PAD is ABI. The doctor will compare the blood pressure in your ankle with the blood pressure in your arm. Your doctor uses a regular blood pressure cuff to get a blood pressure reading and a special ultrasound device to evaluate blood pressure and flow. Doctor will ask you to walk on a treadmill and have readings taken before and immediately after exercising to capture the severity of the narrowed arteries during walking.
- Ultrasound. Doppler ultrasound is a special ultrasound imaging technique that can help your doctor evaluate blood flow through your blood vessels and identify blocked or narrowed arteries.
- Angiography. In this test a dye (contrast material) is injected into your blood vessels to view blood flow through your arteries as it happens. The flow of the contrast material is traced using imaging techniques, such as X-ray imaging or procedures called magnetic resonance angiography (MRA) or computerized tomography angiography (CTA). Another invasive procedure is catheter angiography. It involves guiding a catheter through an artery in your groin to the affected area and injecting the dye that way. This type of angiography, although invasive, allows for simultaneous diagnosis and treatment — finding the narrowed area of a blood vessel and then widening it with an angioplasty procedure or administering medication to improve blood flow.
- Blood tests. Blood tests need to be conducted to measure your cholesterol and triglycerides and to check for diabetes.
Complications
Plaque buildup in blood vessels leading to peripheral artery disease (atherosclerosis) leads to a risk of developing:
- Critical limb ischemia. Beginning of this condition is as open sores that don’t heal, or an injury/ infection of your feet or legs. When such injuries or infections progress critical ischemia occurs and can cause tissue death (gangrene), sometimes requiring amputation of the affected limb.
- Stroke and heart attack. Process of plaque formation and atherosclerosis that causes the signs and symptoms of peripheral artery disease isn’t limited to your legs. Fat deposits also build up in arteries supplying your heart and brain.
Treatment
There are two major goals of treatment for peripheral artery disease. Managing symptoms, such as leg pain, so that you can resume physical activities is the primary goal. To stop the progression of atherosclerosis throughout your body to reduce your risk of heart attack and stroke is the secondary goal.
These goals can be accomplished with lifestyle changes. Quitting the smoking habit is the single most important thing you can do to reduce your risk of complications. You need additional medical treatment if lifestyle changes are not enough. Your doctor may prescribe medicine to prevent blood clots, lower blood pressure and cholesterol, and control pain and other symptoms.